Introduction
Chronic liver diseases (CLD) are very common. Chronic liver diseases represent a major health burden worldwide, with liver cirrhosis being the ninth leading cause of death in Western countries Chronic viral hepatitis B and C, alcoholic liver disease, non-alcoholic fatty liver disease, and hepatocellular carcinoma are the major entities.1 Liver disease accounts for over two million deaths annually (cirrhosis, viral hepatitis, and liver cancer) and accounts for 4% of all deaths worldwide (1 out of every 25 deaths).2 In Africa and Asia, their main causes are viral and parasitic infections, while in Europe and America alcohol abuse is the major cause of liver diseases, although viral hepatitis has increased recently.3 More than 400 million individuals worldwide are chroni- cally infected with hepatitis B virus (HBV), and more than 170 million are chronically infected with hepatitis C virus (HCV).4 A particular type is liver disease that is directly linked to pregnancy and can happen at any point throughout the pregnancy. Another kind is non-pregnancy-related liver illness, which can happen at any time and includes conditions like drug- or virus-induced hepatitis. 5 In the majority of the world, nonalcoholic fatty liver disease (NAFLD) is the most frequent cause of chronic liver disease. 6 The necessity for developing alcohol management techniques at all patient care levels stems from the rising incidence of alcohol use disorder (AUD) along with increases in alcohol-related liver disease (ALD) and other liver diseases.7 Drug-induced liver injur (DILI) can be described as a liver injury caused by a variety of commonly used medications, herbal products.8 Alcoholic liver disease is often to blame for abnormalities in liver function and histopathology in these patients, without taking into account further diagnostic options.9 Alcohol is a major cause of liver cirrhosis in the Western world. The three most widely recognised forms of alcoholic liver disease are alcoholic fatty liver (steatosis), acute alcoholic hepatitis, and alcoholic cirrhosis.10 The highest impact of liver disease is in the young, where it represents the 12th leading cause of DALYs in those aged 25 to 49 years.2
Acute-On-Chronic Liver Failure
Different definitions of ACLF have been proposed in various parts of the world in the past few decades. These include the East Asian APASL criteria, the North American NASCELD definition, and the European European Association for the Study of the Liver - Chronic Liver Failure (EASL-CLIF) definition. These make it difficult to compare and heterogeneous epidemiological data on ACLF. 11 This is a troublesome scenario since different definitions of ACLF cause clinicians to disagree or confusion about how to make the diagnosis. 2 The first consensus definition of ACLF was given by the APASL in 2009, and it was revised in 2014. The primary distinction between this definition and all others is that hepatic insults are only taken into account in cases where they result in liver failure (jaundice and HE). 12
An early decompensation of chronic liver disease accompanied by organ failures and a high short-term mortality rate is characteristic of the syndrome known as acute-on-chronic liver failure (ACLF). The two most frequent underlying liver diseases are alcoholism and chronic viral hepatitis. The most often reported triggering reasons for ACLF include sepsis, active drinking, and return of chronic viral hepatitis in the remaining individuals, accounting for up to 40% to 50% of cases without an identified cause. An excess of systemic inflammation appears to be a major factor in the development of ACLF. For about thirty percent of individuals with ACLF, bacterial infection is the cause of systemic inflammation and the rise of OFs. These patients have ACLF caused on by sepsis. 12 Nearly 50% of ACLF patients in Europe and South Asia had bacterial illness as the ACLF triggering event. 11 About 25% of cases of ACLF are caused by severe alcoholic hepatitis (SAH). It is commonly known that individuals with AIH may experience ACLF. A major issue is still how to treat AIH patients who develop ACLF. 13 Kidney failure and infection are common symptoms, accounting for 35% and 49% of all cases with ACLF, respectively. Within 90 days, the death rate was 58%, with South America having the highest death rates (73%).2 According to the CANONIC study, kidney failure appears to be the most prevalent organ failure globally, accounting for nearly 50% of cases, whereas respiratory failure was the least common, accounting for 11% of cases.11 Hospitalizations for ACLF have risen in the United States during the past decade, and the disorder is associated with a high death rate. Moreover, the expenses for ACLF climbed five times, but they increased two times for cirrhosis. Compared to cirrhosis, the cost per hospitalization for ACLF was 3.5 times greater ($53,570 vs. $15,193). Given the actions required to sustain failing organs and the costs paid after being sent to assisted living facilities or hospice care, the financial load is still very significant. 2 Since there isn't a single, efficient treatment for ACLF patients at present, organ support and management of related problems are the backbone of care.12
Hepatocellular Carcinoma (HCC)
Primary liver cancer is predicted to impact over one million individuals yearly by 2025, making it a difficult global health challenge. The most prevalent kind is hepatocellular carcinoma (HCC), which is becoming more prevalent globally and is primarily brought on by a chronic viral hepatitis B infection. Primary liver cancer ranks second in terms of cancer mortality and is the sixth most frequent type of cancer worldwide. Hepatocellular carcinoma (HCC) is the most frequent histology in the world, accounting for over 80% of cases. 14
The highest rates of both death and incidence in Africa and East Asia (China, Japan, Mongolia, North Korea, South Korea, and Taiwan). Due to the varying frequency of related etiologies, the incidence of HCC varies globally. For instance, 72% of instances occur in Asia, with China accounting for almost 50% of those cases, whereas the incidence in North America is 5%. Mongolia is known for having the highest age-standardized incidence (ASIR per 100,000 people) and mortality (ASMR) rates of HCC in East Asia. Surprisingly, ASIR and ASMR are nearly identical worldwide, demonstrating the significant death rate associated with HCC. North and South America, the Middle East, Oceania, and Northern Europe have the lowest global incidence rates, while Central European nations have intermediate rates. However, there is a lot of variation even within particular geographical areas. For instance, among Asian nations having cancer registries, the ASR for men varies from 2.0 in India's Bhopal and Dindigul to 77.5 in China's Qidong City.14 Hepatocellular carcinoma (HCC) is the most frequent histology in the world, accounting for over 80% of cases. 14 Moreover, HCC ranks seventh among women and fifth among men worldwide in terms of cancer incidence. There is a noticeable disparity in occurrence in practically every country, with male rates two to three times greater than female rates. 14 Estimates from GLOBOCAN show that in 2020, there were 830,180 HCC-related fatalities and around 905,677 new cases. Males had a 2-3-fold greater incidence and fatality rate than females.2
Reduction in hcc worldwid
It has been demonstrated that nations with high rates of HBV immunization have a decrease in the incidence of HCC. HCC has decreased as a result of the last 5-10 years of aggressive HCV treatment. Comprehensive HCC therapy and surveillance programs have also increased survival in some nations. China has implemented targeted public health initiatives to lower aflatoxin exposure and HBV transmission. Japan has similarly experienced a decline in HCV infection rates. The treatment of chronic HBV and HCV, HBV immunization, and public health initiatives to lower aflatoxin exposure are expected to positively affect the incidence of HCC. The primary obstacles still remain in expanding access to these interventions and figuring out who would benefit from antiviral therapy. 2
Drug induced liver injury
Different countries and populations have diverse drug-induced liver injury (DILI) epidemiologies and etiologies. In general, DILI is uncommon in the general population, but it has increased in hospitalized patients, particularly those with unidentified liver disorders. Numerous research offer insightful data regarding the prevalence of DILI. It is important to remember, that it can be challenging to determine the true incidence of DILI and that it might be much greater than what has been reported. 15
31 studies across all were included. Per 100,000 person-years, the overall incidence of DILI was 4.94 (95%CI: 4.05-5.83). According to a time- based cumulative meta-analysis, since 2010, there has been an increase in the incidence of DILI. The incidence differed by region: 1.72 (95%CI: 0.48- 2.95) per 100,000 person-years was the lowest in America, while 17.82 (95%CI: 6.26-29.38) per 100,000 person-years was the greatest in Asia. The findings of every study consistently showed that older adults had a greater incidence of DILI, with equivalent incidence rates for men and women (3.42 vs. 4.64 per 100,000 person-years). In terms of the special drug(s) implicated, the incidence of statin- induced liver injury was 11.30 (95%CI: 6.48-19.69) per 100,000 person-years. In contrast, the incidence varied between 0.16 and 180.97 per 100,000 person- years among patients using antifungal, antidepressant, paracetamol, antidiabetic, anti- tuberculosis, nonsteroidal anti-inflammatory, anti- thyroid, and iron chelator medications. We observed that the general population's worldwide incidence of DILI was 4.94 per 100,000 persons annually, with Asia reporting the highest prevalence when compared to Europe and America. Furthermore, since 2010, the incidence of DILI has increased. The incidence of DILI has increased significantly since 2010, according to a cumulative meta-analysis, with the highest incidence occurring between 2010 and 2020 (15.14 per 100,000 person-years). 16
Alcoholic liver disease (ALD)
(ALD) causes severe morbidity and mortality because to its role as the main reason of cirrhosis, liver cancer, and acute and chronic liver failure. Death.17 Alcohol-related liver disease is a disorder in which alcohol has caused damage to the liver. To acquire the illness, you don't need to be addicted to alcohol; you run the danger of doing so by routinely exceeding acceptable alcohol intake levels. The term "alcoholic liver disease" is occasionally used to describe it, and your doctor may refer to it using the abbreviations used ALD or ARLD.Alcohol-related liver damage has multiple stages.
The most advanced stage of liver disease, cirrhosis, typically takes many years to manifest.Weight loss, jaundice, or yellowing of the skin and eyes, and ascites, or enlargement of the abdomen, are among the symptoms that are often only observed when the diseaseisat a more advanced level.18 About 3.8% of all fatalities worldwide and 4.6% of life years with a handicap are attributed to alcohol usage. Over the past 30 years, liver cancer mortality has decreased in the majority of Western European nations while rising in a number of Eastern European nations, the United Kingdom, Ireland, and Finland.17 Seventy to eighty percent of alcohol- related deaths that are directly reported are caused by liver cirrhosis.80,600 deaths (14,800 deaths for women and 65,900 deaths for men) were linked to alcohol-related liver cancer in 2010. Alcohol-related liver cirrhosis was the cause of 493,300 deaths (47.9% of all liver cirrhosis deaths), or 0.9% of all deaths regardless of the cause (0.7% of all deaths for women and 1.2% of all deaths for men). 10 With the highest rates among men and women in the European Region (14.8% and 3.5%, respectively) and the Americas (11.5% and 5.1%, respectively), alcohol use disorder (AUD) is present in 283 million people worldwide. The countries with the greatest percentage (over 40%) of people aged 15 to 19 who reported heavy drinking were Equatorial Guinea, Gabon, Congo, Estonia, Czech Republic, Ireland, lavita,Lithuania, and Slovenia.2
Epidermatology
According to the Global Burden of Disease Study, the number of deaths from liver disorders has been gradually rising. In 2010, there were about 1 million deaths from liver diseases, or 2% of all deaths worldwide.12 As a result, the years of liver lost (YYL) associated with liver-related conditions surpass those resulting from cancers of the pancreas, oesophagus, stomach, colorectum, and respiratory system combined.variations throughout Europe Considering statistics taken from the World Health Organization's (WHO) mortality database,14 one may calculate that between 60% and 80% of Excessive drinking is the cause of death related to the liver 17. Schistosomial infection is the primary cause of portal hypertension in impoverished nations, while alcohol is the main cause of liver cirrhosis in the Western world. Eighty percent of liver cirrhosis cases that are encountered in UK district general hospitals are related to alcohol. Traditionally, alcoholic cirrhosis was uncommon in nations like Japan and India, but now days it is more frequent 10
The three phases of liver damage caused by alcohol
Alcohol-related fatty liver: The liver will begin to accumulate fat if you consume more than four units of alcohol every day. Alcohol is broken down by your liver, but some of the byproducts are harmful and cause liver damage. In addition to other issues, this causes fat to accumulate in your liver. Your liver may recover if you abstain from alcohol entirely for several months or even years.
Alcohol-related hepatitis: Approximately a third of heavy drinkers that already have alcohol-related fatty liver will eventually progress to this extremely risky stage of the disease. It usually happens after years of binge drinking. However, it can appear abruptly and badly even after you've given up alcohol. It typically occurs after weeks or months of binge drinking, but it can also occur from excessive alcohol consumption over a shorter period of time. This condition, known as acute alcohol-related hepatitis, can lead to severe liver failure.
Cirrhosis: When there is extensive and severe scarring (fibrosis) on the liver, this is the most severe stage of alcohol-related liver disease. One out of every five heavy drinkers will eventually develop cirrhosis. If you suffer one of the more severe types of liver injury, it is imperative that you are referred to a liver specialist. These illnesses require specialised care and are even harder to treat.17
Non-Alcoholic Fatty Liver Disease (NAFLD)
In the United States as well as the rest of the world, nonalcoholic fatty liver disease (NAFLD) is quickly rising to the top of the list of chronic liver disease causes. It is also one of the main causes of cirrhosis, hepatocellular carcinoma (HCC), and liver transplant indications. 19
The global prevalence of non-alcoholic fatty liver disease (NAFLD) grew from 25.3% in 1990– 2006 to 38.0% in 2016–2019, per a recent systematic review and meta-analysis.20 In North America, the prevalence of NAFLD varies from 24 to 48% and is influenced by ethnicity. Although rates may have been underestimated, South America too has high rates (30%). Mexico and Brazil have reported higher prevalences, whereas Canada and Argentina have recorded lower prevalences. According to earlier research, the overall prevalence of NAFLD in Europe was estimated to be between 23% and 33%.The prevalence of NAFLD in the general population varies between European nations; for example, it is highest in Western European nations (e.g., 25%–30% in Germany and the UK) and lowest in Eastern nations (e.g., 20% in Hungary and Romania).According to a recent comprehensive systematic analysis, the overall disease prevalence in Asia is between 28% and 32.4%, with significant regional variations (Japan is 22%, while Iran is 38%). In China, the prevalence risen from 23.8% to 29%. Although there aren't many research conducted in Africa, NAFLD may be 20% more common there. 2
Obesity
The development of cirrhosis and liver cancer in later life is independently associated with obesity throughout the early stages of life, which carries a significant risk of NAFLD. 20 Globally, the prevalence of obesity has more than doubled since 1980, according to the World Health Organization's latest data. Worldwide, around 600 million individuals (13%) and 2 billion adults (39%) are fat or overweight. Over half of all obese people worldwide exist in just ten nations, indicating that the geographic distribution of the disease is unequal. 21 The finding that babies of obese mothers appear to be more likely to have NAFLD—possibly with a more advanced severity—is another unsettling fact. Asia-Pacific region is witnessing an increase in childhood obesity as well. In Asian children, the pooled prevalence of NAFLD was 5.4%, while in teenagers, it was 7.3%. Males had a higher prevalence of NAFLD, which worsened with BMI. In 2002–2010, the prevalence was 4.4%, while from 2010–2020, it was 7.1%. 20 While the majority of NAFLD patients are obese, some are thought to be lean. As was already mentioned, there is a 7% prevalence of lean NAFLD in the US. On the other hand, several Asian nations have greater rates. Lean NAFLD prevalence has been estimated using region-specific BMI thresholds to be 20% in India, 15.2% in Japan, 15% in China, 12% in Greece,12.6% in South Korea, and Iceland. 19
Unheathy DIET
Access to unhealthy foods is closely associated with improvements in socioeconomic position in areas with low or moderate sociodemographic index (SDI).In spite of the rising rates of obesity and type 2 diabetes, the overconsumption of sugar- and fructose-laden foods in Latin America is thought to be the primary cause of NAFLD-related negative outcomes. In other regions of the world, such as Southern Europe, a Mediterranean diet has been accepted as one of the interventions to prevent or treat NAFLD. Ceramides are free fatty acids and lipotoxic substances that may raise the risk of non- alcoholic fatty liver disease (NAFLD) regardless of body mass index and fasting glucose levels. Ceramides are marketed as beneficial for skin care in the West.20
Deaths
Over the period of the last three decades, the total number of deaths among patients with NAFLD has doubled (from 93,757 in 1990 to 168,969 in 2019). However, this increase in mortality may be partially explained by misclassification bias, as deaths previously linked to alcohol may actually have been caused by NAFLD. From 0.10% (0.8%-0.14%) to 0.17% (0.13%-0.23%), the proportion of overall fatalities from all causes related to NAFLD increased. 2
Mortality
Cardiovascular mortality is the leading cause of death for the whole cohort of people with NAFLD.19 due to the intimate relationship that occurs between metabolic syndrome and NAFLD.20 NAFLD patients have a liver-specific mortality rate of 0.77 per 1000 person years, based on reports as well. In people with NASH, this rate is nearly ten times higher. For individuals with liver disease, listing for liver transplantation is a significant outcome in addition to mortality. In this regard, NAFLD/NASH is quickly rising to prominent position in the US as a primary indicator for liver transplantation.19
Viral Hepatatis
The majority of hepatitis cases are caused by five viruses: A, B, C, D, and E. While acute hepatitis can be caused by any hepatitis virus but cirrhosis, increasing liver fibrosis, and an increased risk of liver cancer are most frequently caused by hepatitis B and hepatitis C. Worldwide, the number of deaths from viral hepatitis raised from 980.9 thousand in 1990 to 1412.3 thousand in 2017, and during that same period, the number of DALYs climbed from 35.2 million to 43.1 million. In 2017, 97.6% of all viral hepatitis-related deaths globally have been caused by hepatitis B and C.22 The incidence of HAV, HCV, and HEV infection remain unchanged between 1990 and 2019, although the incidence of acute hepatitis B has decreased, partly because of higher rates of HBV vaccination. In 2020 saw 1.1 million deaths from viral hepatitis B and C-related diseases, which is comparable to the 1.3 million deaths from tuberculosis and far higher than the 0.68 million and 0.627 million deaths from HIV and malaria, respectively. In contrast to the resources allocated to each of the other three infectious diseases, viral hepatitis is being controlled and eradicated globally at a disproportionately lower rate.2 A World Health Organization (WHO) plan to reduce the threat of hepatitis to public health by 2030 was approved by the World Health Assembly. The WHO set this goal at 65% reduced fatalities and 90% reduced new infections.22
Special Consideration
Pregnancy and liver disease
Pregnancy-related liver diseases are significant medical conditions with a serious prognosis that provide difficulties for both hepatologists and obstetricians. It impacts approximately 3% of pregnancies globally and 3-5% of pregnancies in India. It can show up as a number of symptoms, including dark urine, nausea, vomiting, anorexia, yellowish sclera discoloration, and stomach pain etc.
Pregnancy-related liver problems have a serious prognosis that negatively impacts the foeto-maternal outcome, particularly in impoverished nations like India. It is responsible for 60% of perinatal deaths and 14% of maternal deaths. 23
They are classified into two major categories
For gynecologists and hepatologists, a liver disorder is a major pregnancy complication that poses a problem. This could result in a number of perinatal and maternal morbidities, some of which could be fatal for both the mother and the kid. 24
Retrospective Observational Study
Retrospective observational study conducted in a tertiary care center in the Department of Obstetrics and Gynecology at Rajendra Institute of Medical Sciences (RIMS), Ranchi, Jharkhand, India. Patient data admitted between March 2018 and February 2019 was the basis for this study. Out Of the 8264 obstetric hospitalizations that occurred throughout the study period, 126 were identified as pregnant patients with liver Diseases. Preeclampsia, eclampsia, and HELLP syndrome accounted for 59 (46.8%) of the cases in this study, resulting in the most common aetiology for liver diseases. Preeclampsia, eclampsia, and HELLP syndrome were present in 59 instances. 23
COVID -19 and liver diseases
Any liver damage experienced by individuals with or without pre-existing liver disease during the course of COVID-19 treatment is referred to as COVID-19-associated liver injury.25 Even at present, COVID 19 does not primarily affect the liver.2 But there may be abnormal liver damage markers in COVID-19 patients. In 14%–53% of COVID-19 patients, alterations in alanine transaminase (ALT), aspartate transaminase (AST), and elevated bilirubin have been seen.18% of patients with nonsevere and 56% of patients with severe COVID-19 had high serum AST levels, according to a recent study involving 1100 patients.20% of patients with a non-severe COVID- 19 infection and 28% with a severe infection had elevated ALT levels.26 Significantly, liver transplantation lowers the risk of COVID-19 mortality to that of the general population by restoring hepatic function in patients with decompensated cirrhosis. Unfortunately, however, the COVID-19 pandemic has decreased organ donation and liver transplants (from 25% to 80%) in several nations.27 Compared to adults, children who are infected seem to have a milder disease course and a better prognosis. As a result of fact, children with COVID-19 have a special immune response mechanism and unique clinical characteristics.Observing that COVID-19 in children is linked to little or no rise in ALT and AST levels.28
Risk Factors
Patients with cirrhosis had a 1.7-fold increased chance of dying from COVID-19 compared to non-cirrhosis patients, primarily from respiratory failure. 2
In individuals with COVID-19, ALD is independently linked to a 1.8-fold higher risk of mortality.
Compared to COVID-19 individuals without cancer (8%), cancer patients with COVID-19 appear to have a higher chance of dying (39%) or needing invasive ventilation.
Drug-induced liver injury linked to COVID-19 treatments is another potential reason of liver damage in COVID-19 patients.27
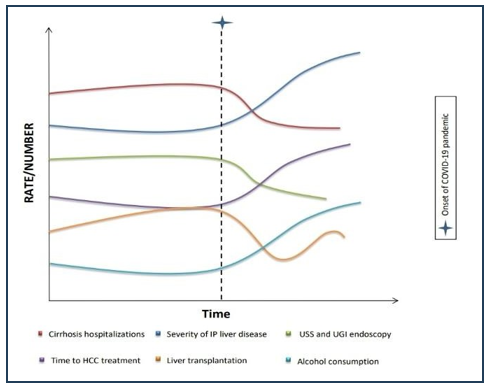
Covid-19 On Hepatology Care
Hepatology services have been significantly impacted by the pandemic. 2 Early in the COVID-19 pandemic, it was reasonable to limit and postpone care for other non-urgent medical illnesses because the prevention, control, and management of SARS- CoV-2-infected patients justifiably occupied center stage.29 According to recent WHO data, among the most commonly interrupted services were those for hepatitis B and C. These consist of services for immunization, testing, treatment, and prevention. It is predicted that a one-year delay in the birth dosage and childhood HBV vaccination will result in 5.3 million more chronic HBV infections in the 2020– 2030 birth cohort and 1 million more HBV-related deaths in these children decades later. 2
Sign and Symptoms
Types of symptoms
Individuals who do exhibit liver illness or damage symptoms may exhibit a variety of symptoms. Among the symptoms you can encounter are encephalopathy, ascites, bleeding varices, and jaundice.
Jaundice (jawn-dis); One common indicator that HCC is being presented is jaundice. According to certain studies, it is present in 28% of African patients when HCC is diagnosed, while it is less common in Chinese, Japanese, or European individuals.30 An eye yellowing is called jaundice. It occurs when your liver can not to properly filter your blood. Your liver function may be declining (becoming worse) or you may have an infection if your jaundice appears out of the blue or gets worse. Make an appointment with your doctor or specialist right once to have it examined.
Bleeding varices (vara-sees); Bleeding varices are bleeding episodes that occur in the stomach or oesophagus (including food pipe). Your liver creates pressure, which causes the blood vessels to enlarge and burst. Bleeding varices are extremely dangerous and could endanger life.Blood in the vomiting or dark, tarry, sticky stools are signs of bleeding varices. In case you suffer any of these signs, you require Quick Medical Help.
Ascites (uh-sigh-teez): An accumulation of fluid in the abdomen (stomach area) is known as ascites. It results from elevated hepatic pressure.It will cause your belly to grow incredibly big. Eating becomes painful since you'll always feel full, and breathing might get difficult, especially if you're lying down. It's possible for some ascites patients to also be malnourished, which occurs when the body doesn't acquire enough nutrients. This is quite dangerous because the ascites fluid can get contaminated. You require URGENT medical attention if you have ascites and experience acute stomach discomfort, fever, and other symptoms.Younger individuals tend to present more frequently with ruptured HCC, hepatomegaly, and discomfort. Ankle oedema and ascites are more common in older patients. 30
Encephalopathy: Non-specific systemic symptoms such as asthenia, anorexia, weight loss, and nausea are common in HCC patients.30 Hepatic cirrhosis symptoms include jaundice, ascites, peripheral edoemas, neurologic indications of hepatic encephalopathy, bleeding, and infections. Other symptoms of hepatic cirrhosis include gynecomastia, palmar erythema, spider angiomas, axillary or chest hair loss, and hypogonadism (testicular shrinkage, loss of libido)
Symptoms and Complications of Cirrhosis
In the initial phases of cirrhosis, there are usually no symptoms. The progressive illness causes symptoms such as lack of appetite, drowsiness weight loss, abdominal pain, spider-like blood vessels, and intense itching 31
Paraneoplastic Syndrome
Hypolycemia
Hypercalcemia
Erythrocytosis
Thrombocytosis
Arterial hypertension
Diarrhea.32
Diagnosis
A liver biopsy may assist recognise NAFLD if clinical, serologic, or biochemical tests indicate that it could be a differential diagnosis. Autoantibodies27, higher iron indices, recent drug changes, and lack of visible hepatic steatosis on cross-sectional imaging are signs of such conditions. 33
Serological tests
Due to limitations in liver biopsy, non-invasive techniques for detecting liver fibrosis were developed. According to Afdhal and Nunes et al., the ideal marker for liver fibrosis should meet the following criteria: The test should be liver-specific, independent of liver, renal, or reticulo-endothelial function, measure one or more fibrosis-related processes (stage, matrix deposition, or matrix removal), and be simple to administer.
Radiological tests
Ultrasound (US), computed tomography, and magnetic resonance imaging (MRI) are standard examination methods that can yield specific findings, but their sensitivity is quite restricted because major structural changes are only apparent in advanced CLD. Consequently, there have been constant efforts to look for improvements in technology.
Perfusion examinations
Liver stiffness measurement
Real-time elastography
Magnetic resonance elastography.
Double contrast material-enhanced MRI4
Imaging techniques
Hepatic steatosis can be diagnosed by ultrasound, magnetic resonance imaging (MRI), and computerised tomography (CT) scan. The most popular and affordable technique for diagnosing mild to severe steatosis is ultrasonography.
Technically, a volume of interest is established and coronal, axial, and sagittal pictures of the liver are obtained, avoiding the main blood vessels and bile ducts. 34
The following are the blood tests that are most frequently carried out:
Test for serum bilirubin: This test determines the blood's bilimibin levels. Bilirubin is produced by the liver and excreted in bile.Increased bilirubin levels might be a sign of a bile duct blockage or an issue with the liver's bile processing.
Test for serum albumin: This test helps diagnose liver disease by determining the amount of albumin, a protein, in the blood.
Serum alkaline phosphatase test: This test gauges the blood's concentration of the enzyme alkaline phosphatase. Although alkaline phosphatase is present in many tissues, the liver, biliary system, and bone have the largest quantities.This test can be used to identify liver lesions like tumours or abscesses that may cause biliary obstructions as well as to assess liver hanctioning.
Prothrombin time test (PTT): This test evaluates the amount of time needed for blood to clot. The production of a protein by the liver and vitamin K are necessary for blood clotting. Extended bleeding could be a sign of liver illness or other deficits in certain clotting factors.
Alanine transaminase (ALT) test: quantifies the amount of the liver-specific enzyme alanine aminotransferase that is released into the bloodstream following acute liver cell injury. This test may be carried out to evaluate the therapy of acute liver disease, such as hepatitis, or to look over liver function.
Test for aspartate transaminase (AST): This test determines the amount of this enzyme, which is released into the circulation to affect liver or cardiac issues, and is present in the liver, kidneys, pancreas, heart, skeletal muscle, and red blood cells.
Test for lactic dehydrogenase: This test helps diagnose liver illness and can identify tissue damage. One kind of protein, known as an isoenzyme, that is involved in the body's metabolic process is lactic dehydrogenase 35.
Prevention
Refrain from coming into touch with the bodily fluids and blood of others.
Food should be stored safely.
Use aerosol sprays with caution.
Protect your skin.
Get a vaccination 36
Treatment
Therapy of hepatitis
Hepatitis A is one of the best examples for vaccine preventable infectious diseases in the world with several options for vaccination.1992 saw the release of HavrixTM, the first hepatitis A vaccination that was proven to be successful. 37 Combination vaccinations for hepatitis A and B are now accessible as TwinrixTM from GlaxoSmithKline GmbH & Co. KG, 80700 Munich, Germany.
Drugs for HBV Treatment
Drugs for HCV Treatment
The distinct RNA virus known as the hepatitis D virus (HDV) needs a helper function that is supplied by As a result, HDV can only spread among HBV- positive individuals. The hepatitis D infection's clinical course is more treatment should always be started since its severity is greater than that of other hepatitis viruses. Regretfully, there is currently no proven treatment for hepatitis D infection.About 30% of treatments with interferon therapy are linked with therapeutic success. 36
Since there is not currently a viable treatment for NAFLD, weight loss accomplished through various methods—including diet, exercise, anti-obesity drugs, and bariatric surgery—has been pushed as the accepted course of care. 1
Glycyrrhizina
Stronger Neo-minophagen C (SNMC), a standardised extract comprising glycyrrhizin, cysteine, and glycine, has been established as a therapy for chronic hepatitis (Hidaka et al., 2007). Galactosamine (D-GalN) and lipopolysaccharide (LPS)-induced fulminant hepatic failure can be successfully prevented by SNMC.
Picrorhiza kurroa
In the Ayurvedic medical system, Picrorhiza kurroa Royle Benth. (Scrophulariaceae) is a well-known plant that has been traditionally used to treat upper respiratory tract and liver diseases.
Resveratrol
MDA in the liver was evaluated as an indicator of oxidative stress. After 14 days, a significant resveratrol buildup was discovered in the liver. After one week, the increase in MDA liver levels brought on by the CCl4 injection was reduced by 63% with resveratrol treatment. 1
Conclusion
Many professionals who deal with substance abuse may not fully understand the complexity of liver illness.However, for problem drinkers, liver disease is a frequent and significant source of illness and mortality.Problem drinkers' liver damage may be exacerbated or brought on by liver illnesses other than alcoholism.Professionals in primary care and drug abuse should possess the necessary knowledge and abilities to recognise and evaluate alcoholic liver disease.Even in cases of advanced or end-stage liver disease, quitting or cutting back on drinking improves the prognosis from alcoholic liver disease.In addition to quitting or consuming less alcohol, there is effective treatment for severe alcoholic liver disease and associated sequelae.Early-life obesity is associated with a high risk of nonalcoholic fatty liver disease (NAFLD), which progresses to cirrhosis and cancer and accounts for most liver disease-related deaths.