- Visibility 60 Views
- Downloads 8 Downloads
- DOI 10.18231/j.ijpca.2023.046
-
CrossMark
- Citation
Knowledge, attitude and practice of self-administered insulin by diabetes mellitus patients: A cross sectional study
- Author Details:
-
Akshay Hasmukhbhai Parmar *
-
Anupama Sukhlecha
-
Kajal Jasubhai Katariya
Introduction
Diabetes mellitus (DM) is a group of common metabolic disorders that share the phenotype of hyperglycaemia.[1] The pathogenesis of DM is contributed by both genetic and environmental factors that involve insufficient insulin secretion, insulin resistance, increased glucose production, and/or fat and protein metabolism abnormalities.[2] Patients with diabetes are at high risk of cardiovascular, peripheral vascular, and cerebrovascular disease.[3] These complications can be prevented with appropriate and judicious medical care.[4]
India is emerging as the world’s diabetic capital. Type 1 DM is the result of complete or near-total insulin deficiency. Type 2 DM is a heterogeneous group of disorders characterized by variable degrees of insulin resistance, impaired insulin secretion, and increased glucose production. Insulin is mandatory for type 1 diabetes and is frequently required in type 2 diabetes as the disease progresses. Statistics from developed countries show that more than 30% of all diabetics use insulin either singly or in combination with oral anti-diabetic drugs (OADs).[5]
Inadequate awareness regarding insulin use is likely to influence its acceptance and adherence. Being an injectable drug, its use is more likely to be influenced by misconceptions than OADs. There are several Indian studies with an emphasis on diabetes epidemiology.[6] It’s imperative that all diabetic patients who use insulin be educated about its use.[4] Many studies have been published in India on diabetes epidemiology. However, knowledge, attitude, and practice (KAP) surveys of insulin use in diabetic patients are limited. Thus, the present study was conducted with two objectives: to assess the extent of insulin literacy in all adult diabetics, irrespective of whether they are using insulin, and to assess, in actual insulin users, the extent to which they follow accepted practice at tertiary care teaching hospital.
Materials and Methods
A single-centric, cross-sectional KAP study was carried out among diabetes mellitus patients attending the medicine out-patient departments (OPD) at a tertiary care teaching hospital. The study was cleared by the Institutional Ethics Committee (IEC no. 72/01/2023). The study participants were adults (>18 years old) with type 1 or type 2 diabetes mellitus (DM) who were willing to respond to the study questionnaire. The sample size was 166, which was calculated using the formula n = z2*p(1-p)/e2, where z is the z score (1.96), p is the population proportion (50%), e is the margin of error (8%) at a 95% confidence interval, and 10% are nonresponders.[7] Written informed consent was obtained prior to giving them a questionnaire in a language they could best understand. The questionnaire used for the survey was designed by the authors and underwent validation by pharmacologists at our institute. The finalised questionnaire had 28 items, of which the first 11 pertained to knowledge. The remaining (17 items) focused on attitude and practice, and this section was administered only to current insulin users. The duration of the study was 6 months. Information of all the participants was kept confidential throughout the study period. The results were analysed based on the responses and expressed as percentages. All data were analysed using Microsoft Excel software.
Results
Out of 166 patients who were given questionnaire, 151 completed the questionnaire and were included in analysis. Sociodemographic data of these 151 patients has been presented in [Table 1].
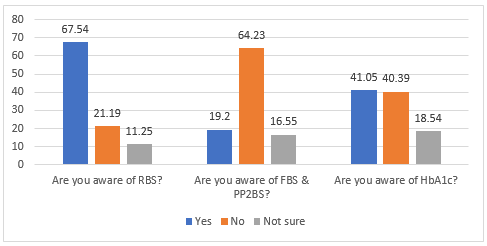
Responses of the patients towards knowledge of self-administered insulin (n=151) are presented in [Table 2]. Out of total 151 patients, only 62 (41.1%) were aware of HbA1c (a test for assessing long-term blood sugar control). ([Figure 1])
Out of total 151 patients who were on anti-diabetic drugs, only 81 (53.6%) were prescribed insulin.
Responses of the patients towards attitude of self-administered insulin (n=81) are presented in [Table 3].
Responses of these insulin users (n=81) towards practice of self-administered insulin are presented in [Table 4].
|
Variables |
|
N (%) |
|
Gender |
Male |
58 (38.41) |
|
Female |
93 (61.58) |
|
|
Age groups (years) |
<60 |
103 (68.21) |
|
≥60 |
48 (31.78) |
|
Questions on knowledge |
Response |
N (%) |
|
Do you think insulin can cure diabetes? |
Yes |
148 (98.01) |
|
No |
3 (1.98) |
|
|
Are you aware that there are different types of insulin? |
Yes |
100 (66.22) |
|
No |
51 (33.77) |
|
|
Are you aware that there are different types of insulin delivery devices? |
Yes |
48 (31.78) |
|
No |
97 (64.23) |
|
|
Not sure |
6 (3.97) |
|
|
Are you aware of RBS (a test for assessing long term blood sugar control)? |
Yes |
102 (67.54) |
|
No |
32 (21.19) |
|
|
Not sure |
17 (11.25) |
|
|
Are you aware of FBS & PP2BS (a test for assessing long term blood sugar control)? |
Yes |
29 (19.20) |
|
No |
97 (64.23) |
|
|
Not sure |
25 (16.55) |
|
|
Are you aware of HbA1c (a test for assessing long term blood sugar control)? |
Yes |
62 (41.05) |
|
No |
61 (40.39) |
|
|
Not sure |
28 (18.54) |
|
|
Do you know what is glucometer? |
Yes |
79 (52.31) |
|
No |
61 (40.39) |
|
|
Not sure |
11 (7.28) |
|
|
Do you know the complications of diabetes? |
Yes |
72 (47.68) |
|
No |
66 (43.70) |
|
|
Not sure |
13 (8.60) |
|
|
Do you know symptoms of Hypoglycaemia? |
Yes |
132 (87.41) |
|
No |
19 (12.58) |
|
|
Do you carry simple carbohydrates (candy, sweet biscuit) with you while travelling? |
Usually |
68 (45.03) |
|
Sometime |
68 (45.03) |
|
|
No |
15 (9.93) |
|
|
Do you believe bitter condiments can be used to control blood sugar? |
Yes |
110 (72.84) |
|
No |
29 (19.20) |
|
|
Not sure |
12 (7.94) |
RBS=Random blood sugar, FBS=Fasting blood sugar, PP2BS= post-prandial (2 hours after having a meal) blood sugar, HbA1c= Glycated haemoglobin
|
Questions on attitude |
Response |
N (%) |
|
Are you self-confident about self-administration of insulin? |
Strongly Agree |
40 (49.38) |
|
Agree |
29 (35.80) |
|
|
Unsure |
10 (12.34) |
|
|
Disagree |
2 (2.46) |
|
|
Insulin can be administered even if the vial is having clumps |
Agree |
4 (4.93) |
|
Unsure |
5 (6.17) |
|
|
Disagree |
44 (54.32) |
|
|
Strongly Disagree |
28 (34.56) |
|
|
Insulin should not be administered at the same site |
Strongly Agree |
35 (43.20) |
|
Agree |
30 (37.03) |
|
|
Unsure |
4 (4.93) |
|
|
Disagree |
12 (14.81) |
|
|
Too high or too low insulin can cause drastic alterations in blood glucose |
Strongly Agree |
24 (29.62) |
|
Agree |
46 (56.79) |
|
|
Unsure |
3 (3.70) |
|
|
Disagree |
4 (4.93) |
|
|
Strongly Disagree |
4 (4.93) |
|
|
Insulin can be stopped once blood glucose is controlled |
Agree |
20 (24.69) |
|
Unsure |
3 (3.70) |
|
|
Disagree |
56 (69.13) |
|
|
Strongly Disagree |
2 (2.46) |
|
|
Once insulin is started, diet and exercises are not needed |
Agree |
3 (3.70) |
|
Disagree |
50 (61.72) |
|
|
Strongly Disagree |
28 (34.56) |
|
Questions on practice |
Response |
N (%) |
|
Where do you inject insulin? |
Upper arm |
61 (75.30) |
|
Abdomen |
20 (24.69) |
|
|
Do you clean the injection site with spirit beforehand? |
Yes |
39 (48.14) |
|
No |
42 (51.85) |
|
|
After introducing the syringe, do you withdraw it partly to look for presence of blood? |
Yes |
2 (2.46) |
|
No |
79 (97.53) |
|
|
Where do you store your insulin vial? |
Refrigerator outer compartment |
79 (97.53) |
|
Not fixed |
2 (2.46) |
|
|
Do you rotate sites? |
Yes |
55 (67.90) |
|
No |
26 (32.09) |
|
|
When do you take insulin in relation to your meals? |
Just Before meals |
79 (97.53) |
|
Not Fixed |
2 (2.46) |
|
|
Do you skip food after taking insulin? |
Sometime |
36 (44.44) |
|
No |
45 (55.55) |
|
|
Do you miss insulin doses? |
Yes |
67 (82.71) |
|
No |
14 (17.28) |
|
|
Do you check your blood sugar level at home using glucometer? |
Yes |
21 (25.92) |
|
No |
60 (74.07) |
|
|
Do you regularly get your fasting/post meal blood sugar level checked in a laboratory? |
Yes |
20 (24.69) |
|
No |
61 (75.30) |
|
|
Are you getting treatment for complication of diabetes? |
Yes |
2 (2.46) |
|
No |
77 (95.06) |
|
|
Not sure |
2 (2.46) |
Discussion
The diabetes epidemic is spreading around the globe with the help of rising urbanisation, rural-to-urban migration, sedentary lifestyle adoption, and bad eating practises. These unfavourable conditions combine with Indians' already high hereditary risk for diabetes to cause diabetes to manifest earlier in life.[8] In addition to dietary and lifestyle changes, the administration of insulin or other anti-diabetic medications, ongoing education and counselling efforts are necessary for the management of this complicated metabolic condition. The need for insulin is all the more acute among diabetics to ensure its effective and safe use. In order to gather information on self-administered insulin, our KAP study was designed in this context. As far as knowledge and attitude are considered, the study population showed satisfactory trends comparable to earlier KAP studies conducted in other parts of India.[9], [10]
Approximately 148 (98%) of our subjects had a satisfactory idea about how insulin can cure diabetes. Similar findings were found in the studies conducted by Shah V et al.[6] Around 100 (66.2%) were aware of different types of insulin, and 48 (32%) knew about different types of insulin delivery devices. Only 62 (41.1%) were aware of HbA1c (a test for assessing long-term blood sugar control). ([Figure 1]) Despite knowledge of hypoglycaemia symptoms 132 (87.4%), only 68 (45%) carried simple carbohydrates with them while travelling. The result was supported by the study conducted by Choudhury SD et al.[5] Overall, in our study, awareness regarding insulin as a therapeutic option was satisfactory.
According to our study, the diabetic patients’ attitude towards insulin self-administration was favourable 69 (85.2%). Study conducted by Fego et at. also shown similar finding. [11] Around 35 (43.2%) strongly agreed, and 30 (37%) agreed that insulin should not be administered at the same site. This was supported by study conducted by Asmelash D.[12] The majority of patients 70 (86.4%) agreed that too much or too little insulin can cause drastic alterations in blood glucose.
Around 81 (53.6%) current insulin users, 61 (75.3%) inject insulin in the upper arm, and 20 (24.7%) inject in the abdomen. The majority of the respondents, 55 (67.9%), used to rotate the injection site after taking insulin, and 39 (48.1%) used to clean their injection site with spirit beforehand. Similar result found with study done by Binu Mathew et al. in which 77.1% patients rotate injection site. [13] Missing doses in insulin therapy was reported by 67 (82.7%) of the patients. Only 21 (25.9%) used glucometers regularly; the majority had never used one.
Information and education, which increase knowledge, attitude, and practice, are crucial components of comprehensive diabetes treatment. There are numerous ways to accomplish this, such as by displaying audio and video continuously while patients are waiting for consultations, The patient could be given a booklet with illustrations containing information on the various types of insulin and their color-coding, the locations and methods for administering it, how to store it, symptoms of hypoglycaemia and hyperglycaemia, complications of insulin, and how to manage them. This might help the patients have a better understanding of self-administration of insulin and also improve their practice skills.
Conclusion
Knowledge and attitude were good in the majority of patients, but practice regarding the use of insulin was poor. Skilled health care providers could educate diabetes mellitus patients on self-care management and insulin self-therapy and bridge this gap.
Source of Funding
None.
Conflict of Interest
None.
References
- DL Kasper, MD William Ellery, DL Kasper. . Harrison’s principles of internal medicine. 2015. [Google Scholar]
- LL Brunton, BC Knollmann. . Goodman & Gilman’s the pharmacological basis of therapeutics 2023. [Google Scholar]
- KG Alberti, PZ Zimmet, W Consultation. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus. Provisional report of a WHO Consultation. Diab Med 1998. [Google Scholar]
- UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998. [Google Scholar]
- A Hazra, S Choudhury, S Das. Survey of knowledge-attitude-practice concerning insulin use in adult diabetic patients in eastern India. Indian J Pharmacol 2014. [Google Scholar]
- V Shah, P Kamdar, N Shah. Assessing the knowledge, attitudes and practice of type 2 diabetes among patients of Saurashtra region, Gujarat. Int J Diab Dev Ctries 2009. [Google Scholar]
- MA Pourhoseingholi, M Vahedi, M Rahimzadeh. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench 2013. [Google Scholar]
- CP Raj, M Angadi. Hospital-based KAP study on Diabetes in Bijapur. Karnataka Indian J Med Spec 2010. [Google Scholar]
- HB Chandalia. . Rssdi Textbook of Diabetes Mellitus 2014. [Google Scholar]
- A Ramachandran, C Snehalatha, A Kapur, V Vijay, V Mohan, AK Das. High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia 2001. [Google Scholar]
- MW Fego, JT Yasin, GM Aga. Knowledge, Attitude and Practice Towards Insulin-Self Administration Among Diabetic Patients Attending Bedele Hospital, Southwest Ethiopia, 2019/2020. Diabetes Metab Syndr Obes 2019. [Google Scholar]
- D Asmelash, N Abdu, S Tefera, HW Baynes, C Derbew. Knowledge, Attitude, and Practice towards Glycemic Control and Its Associated Factors among Diabetes Mellitus Patients. J Diab Res 2019. [Google Scholar] [Crossref]
- B Mathew, EA M Reddy, SS Antin, A Balkees, H Doddayya. Assessment of knowledge, attitude and practice of insulin therapy among diabetes patients. Int J Curr Res 2019. [Google Scholar]
