Introduction
Good medical health care facility in the rural part of India is not yet available in all parts of the country. Maternal health is very important and is always considered as important as two lives are involved. In developing and underdeveloped countries, lack of medical facilities and early diagnosis and treatment is one of the major contributing factors. Lack of education among the population is also an important contributing factor to maternal mortality. Various diseases related to maternal mortality are anemia, hemorrhagic complications, and other infections are common. The government of India has taken various steps to provide maximum care to pregnant females and to reduce maternal mortality.1 Involvement of primary health care system at rural level, visiting door to door and keep doing surveys and identify the pregnant women is done on regular basis. The Asha health care worker and anganwadi workers take maximum responsibilities. The government of India has not only supported health but also for nutrition, vaccination and financial supports are provided to the pregnant women. Most of the rural Indian populations are working as a farmer or belongs to the farming population. Agricultural related health issues are not uncommon among pregnant women due to exposure. This study aimed to know what type of maternal patients was admitted to the medical critical care unit of our rural tertiary care hospital and their overall outcome.
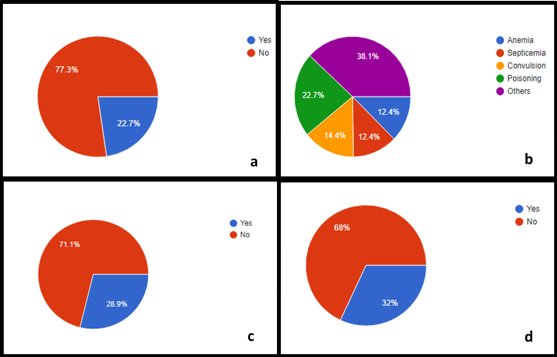
Figure 1
(a) Age wise distribution, (b) Gravida wise distribution, (c) Antenatal registration status, (d) Registered as medico legal cases
Materials and Methods
This retrospective study was conducted in a rural tertiary care hospital with a facility of 40 beds and caters to all types of emergency services. The data collection was done for two years i.e 1st January 2020 till 31st December 2021. Patients aged more than 18 years, either with antenatal or postnatal period having medical problems requiring critical care admission, are included. Any patients who were referred from outside hospitals are not included in this study. Patients requiring any surgical critical care services are excluded from this study. A total of 97 patients were part of this study. The type of admission, gravida, duration of ICU stay, whether they were registered as medico-legal cases, whether the patients were registered cases for antenatal care, type of disease, need of ventilation, treated or referred or discharged against medical advice, and overall outcome and death were recorded.
Results
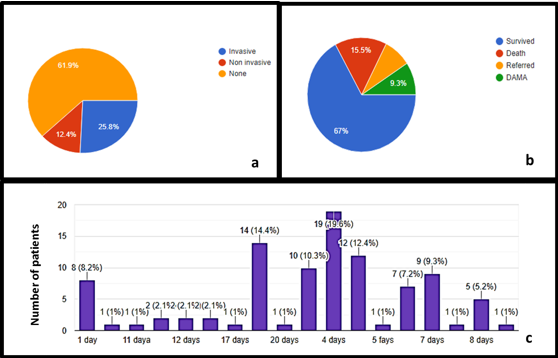
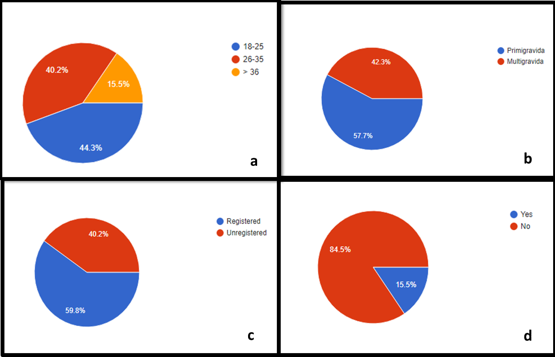
A total of 97 patients were admitted during the period mentioned above. Various age groups of patients were admitted. The maximum number of patients were aged between 18-25 years, 43(44.3%) of patients. There were 15(15.5%) patients whose age was more than 35 years. Among 97 patients, 56 (57.7%) were primigravida, and 58(59.8%) of the patients were registered antenatal cases. 82(84.5%) of cases were registered under the medico-legal case as per Indian law. 68(70.1%) patients had lower segment cesarean sections. Among 97 patients, 22(22.7%) of patients had comorbid illnesses. A total of 22(22.7%) patients got admitted for poisoning-related issues, which was the single most common cause among 97 admissions. 25(25.8%) of patients were on invasive mechanical ventilation and 12(12.4%) were on noninvasive mechanical ventilation. The average number of critical care unit stay was 4 days. 65(67%) patients survived and 15(15.5%) patients died, while 17(17.52%) patients either took discharge against the advice or were referred. (Fig 1- 3)
Discussion
Management of critically ill obstetric patient’s remains challenging due to the physiological changes occurred due to pregnancy.2, 3 Maternal healthcare is very challenging in rural area as two important factors may hinder it, viz, the availability of healthcare set up and lack of awareness.4 In our rural area, the hospital caters various emergency services to all type of patients. Undoubtedly, the obstetric patients admitted in our hospital were of age group between 18 and 25 years age group. This could be due to practice involved among rural population that is early marriage. More than 50% of the patients were primigravida patients and also were registered antenatal cases. This shows that there is an awareness of health care facility, however there is a lot of scope to improvise the need of antenatal case registration and education by the government. Although various level like primary healthcare workers, Asha workers and anganwadi workers are trying to reach the pregnant women and deliver the best service, unfortunately all patients were not covered.5, 6 The government should consider registration of all pregnant women as one of the mandatory criteria for free services. Although the government is providing monitory benefit which is very minimal considering the inflation. In our study, the admission of primigravida patients was more. There is no scientific or social cause to explain it.
The maternity patients who had various medical disorders and were in need of medical line of management got admitted in our hospital. The number of organophosporus poisoning patients was quite high, i.e around 22, and it was the single most common cause among 97 patients. The consumption of the insecticide or exposure to the insecticide while working in the field may the cause for it. Since the insecticides are easily available in the rural area, this might be the most common problem which has been seen. Although many patients due to social reason the reasons given as accidental exposure the reality is different. Domestic violence among pregnant females is not uncommon. We tried to collect the information for the poisoning, but based on clinical practice the reasons mentioned by the patient or patient relative was not accurate, hence we omitted this from the study. Patients were not only had organophosporus poisoning but also for non organophosphorus poison. In our study, the majority of the patients who got admitted were related to medico-legal case. Since we had the large number of organophosporus patients, this might be one of the reasons to see. There were other medico-legal related cases like snake bite, especially during monsoon season. Since we studied among the rural patients it is not uncommon to see the snakebite related patients. The majority part of the population surrounding to this area is related to agriculture the snake bite or other insect bite is not uncommon. The incidence or the trend of admission with history of snakebite was most common during monsoon season. Nearly 75 patients had comorbid illness like diabetes or hypertension. Some of the patient got admitted with history of viral fever and gastroenteritis. Various other disorders like convulsion, severe anemia and septicemia patients were also seen. The hygiene and its importance among rural population are very poor. The government should initiate projects to deliver safe and hygienic water which is a basic need. Early diagnosis and treatment of the complicated cases or viral fever is very important and saves the life of the patient. There should be a check list and should be made mandatory for all primary healthcare workers that early referral of the patient to higher centers. Safe transportation is one of the major challenges in rural area. Although the government is putting lot of effort to improve this, authors recommend having a dedicated ambulance facility for rural area. The ambulance should be equipped well with well manned. The person working under ambulance should have minimum basic knowledge about the resuscitation. Most importantly the ambulance services should be made free of cost. There should be a rule by the government that dedicated beds should be allotted in any tertiary care hospital. The government should come up with dedicated obstetric tertiary care hospitals at district level which can cater for both medical and surgical related diseases. Since the patients admitted in the medical ICU were seen with medical cause, the blood or blood product related transfusion was very less and transfused for 31 patients. Most of the patient who received blood or blood products are anemia, snakebite or septicemia related patients. Nutritional anemia is very common among rural Indian population. Pregnant woman due to their physiological changes the nutrition requirement increases from trimester to trimester. Prevention of anemia among rural population is very challenging. Nearly 25 patients received invasive ventilator therapy, while 12 patients received noninvasive ventilation as a treatment part. These patients were either had pneumonia or multiorgan failure due to septicemia. Community acquired pneumonia is very common among pregnant females.7, 8 In our study we did not collected the data of the obstetric patients who suffered with covid infections as there was a dedicated covid hospital. Most of the patients had community acquired pneumonia. On an average, majority of the patients stayed for 4 days in the ICU, minimum was 1 day and maximum was 8 days. Most of the patients who had asymptomatic snake bite might have been discharged from the ICU in a day against medical advice.
Majority of the patients (67%) survived and got shifted out of the ICU, while 9.3% of the patient took discharge against medical advice. It is important to mention here that, although we studied about obstetric patients admitted in medical critical care we understood that the good outcome depends upon the multidisciplinary approach.9 Irrespective of the type of the disease the patients were referred for obstetric examination to understand the maternal and fetal wellbeing.
We observed that nearly 15patient died during the course of the treatment. Most of the patients were related to organophosporus consumption or due to multiorgan failure. It is not uncommon to see the pregnant patients with OPP poisoning especially in developing countries.10 One of the reasons for such high mortality is lack of awareness among rural people, delayed hospitalization and poor transportation. Although organophosporus poisoning is a treatable condition it is important to note here that one should reach the hospital to the earliest. The outcome of the patient depends upon early diagnosis and early initiation of the treatment.
Limitation of the Study
This is a single center study, thus there is a need of multi-centric study. This study is a retrospective study but it is ideal to consider prospective study so that detailed information can be collected.
Conclusion
Obstetric patient admission in the rural critical care unit is not uncommon, and poisoning is the most common cause of admission in the medical critical care unit, hence it is the responsibility of the local leaders, healthcare workers and government body to educate them. A good healthcare set up over and above the primary health care should be considered.