Introduction
Vomiting or emesis, is defined as the involuntary, forceful expulsion of the contents of stomach through the mouth and sometimes from nose.
Types of Vomiting
Features of Cancer Chemotherapy induced nausea and vomiting:
Acute emesis: which can feature within 24 hrs of treatment.
Delayed emesis: within 1-7 days after treatment (rare & most commonly associated with cisplatin).
Anticipatory emesis: occurs before administration of chemotherapy; it reflects a conditioned response to stimuli such as sight & smell.
Breakthrough: Nausea and/or vomiting that occurs within 7 days post chemotherapy.
Refractory: Nausea and/or vomiting that occurs in subsequent chemotherapy cycles despite maximum antiemetic protocol
Anticipatory: Nausea and/or vomiting that is triggered by sensory stimuli associated with chemotherapy administration.1
Table 1
Causes of vomiting2
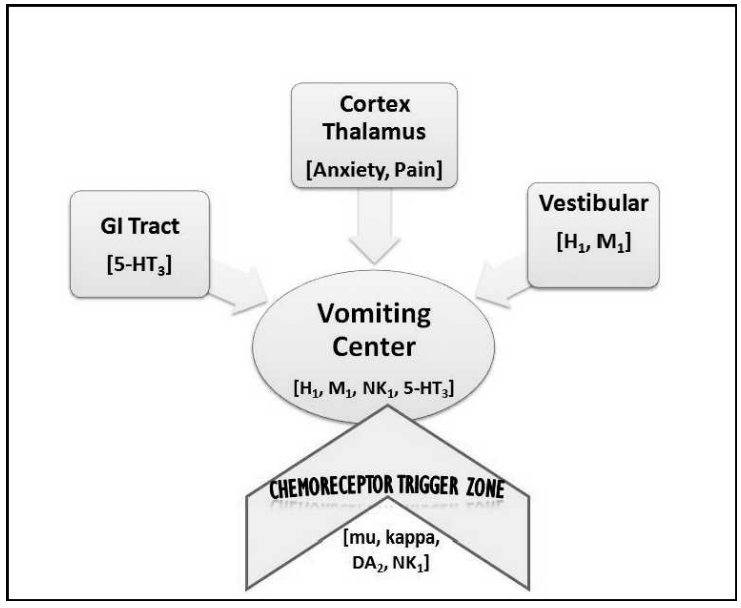
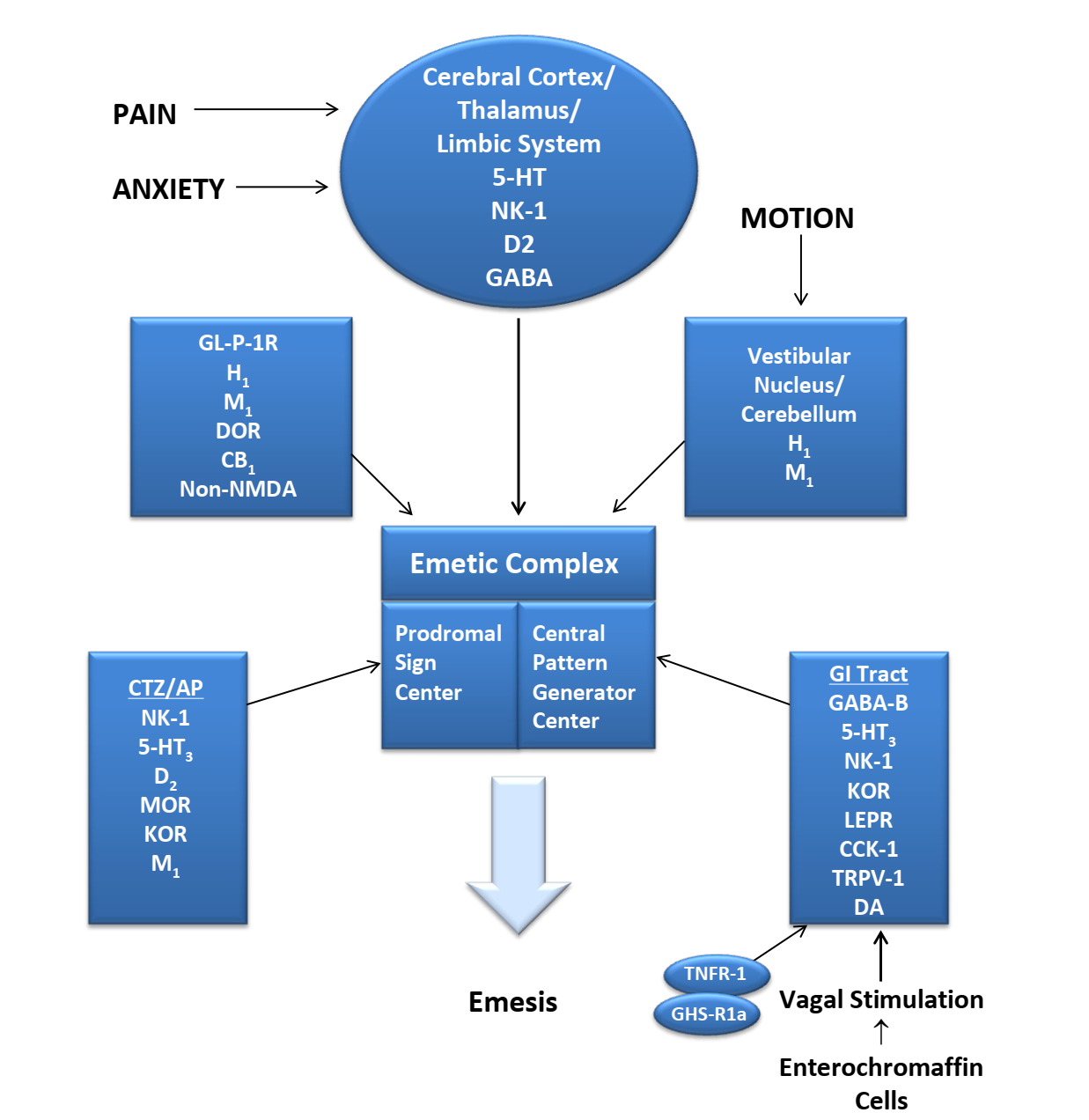
Vomiting centre
The chemoreceptor trigger zone in the Area postrema plays a crucial role in emesis and is one of principal areas that can induce emesis. The other sites besides the CTZ that relay information to the vomiting center to induce emesis include the GI tract, the vestibular system, and the higher centers in the cortex and thalamus.
Vomiting is through a complex series of multi-afferent neural pathways involving the some neuro-transmitters - 5HT3, serotonin, dopamine, histamine and acetylcholine. Drugs that block these receptors have useful anti-emetic properties. Antagonists of histamine and acetylcholine are more useful in controlling vomiting associated with motion sickness, whereas serotonin receptor antagonists (ondansetron) and dopamine receptor antagonists (metoclopramide) are more useful in controlling chemotherapy induced emesis.3
Table 2
Emetogenic potential of anticancer drugs
Table 3
Classification of antiemetic drugs
Antiemetic Profile
Substance P and antagonist
Substance P belongs to tachykinin family and acts as a neurotransmitter. Substance P is found in the gut and the central nervous system, specifically the vagal afferent fibers that innervate the nucleus tractus solitarii and the area postrema. Substance P binds to a specific neurokinin 1 receptor (NK1). Substance P applied directly to the nucleus tractus solitarii produced emesis.
Aprepitant is a highly selective antagonist of the G-protein coupled neurokinin-1 receptor. Aprepitant has little or no affinity for serotonin (5-HT3), dopamine, and corticosteroid receptors, the targets of existing therapies for chemotherapy-induced nausea and vomiting (CINV) and postoperative nausea and vomiting (PONV). Neurokinin-1 receptors are present in both the central and peripheral nervous systems. Their primary ligand is substance P, a nociceptive neurotransmitter. The areas in the brainstem thought to play critical roles in the vomiting reflex are the central pattern generator, the nucleus tractus solitarius (NTS), and area postrema. Aprepitant (oral) and fosaprepitant (intravenous prodrug) are indicated for the prevention of nausea and vomiting.
The recommended dose of Aprepitant is 125 mg orally 1 hour prior to chemotherapy treatment (Day 1) and 80 mg orally once daily in the morning on Days 2 and 3.)
Fosaprepitant dimeglumine, is a prodrug of aprepitant, was developed to provide a parenteral alternative to the orally administered aprepitant. Fosaprepitant is rapidly converted to aprepitant via the action of ubiquitous phosphatases. Based on equivalence studies, 115 mg fosaprepitant seems to be the substitute for 125 mg orally administrated aprepitant
Dose of (fosaprepitant dimeglumine) for Injection may be substituted for oral Aprepitant (125 mg) on Day 1 only as part of the CINV regimen.4, 5
Rolapitant is a selective and competitive antagonist of human substance P/NK1 receptors with antiemetic activity. Rolapitant is indicated in combination with other antiemetic agents in adults for the prevention of delayed nausea and vomiting associated with initial and repeat courses of emetogenic cancer chemotherapy, including, but not limited to Highly emetogenic chemotherapy. The recommended dosage of rolapitant is 180 mg (two 90-mg tablets) administered orally as a single dose one to two hours prior to the start of chemotherapy on day 1 with or without food. Rolapitant is well tolerated, constipation, headache, fatigue, dizziness, dyspepsia, hiccups, and neutropenia have been observed in treated patients.6
5HT3 receptor antagonists
Selective serotonin receptor (5-HT3) antagonists block serotonin both peripherally, on gastrointestinal (GI) vagal nerve terminals, and centrally in the chemoreceptor trigger zone. This blockade results in powerful antiemetic effects. 5-HT3 receptor antagonists may ameliorate nausea/vomiting in a number of circumstances and have been utilized as important antiemetics for multiple conditions such as chemotherapy-induced nausea/vomiting (CINV), radiation-induced emesis (RIS), and postoperative nausea/vomiting (PONV).
Table 4
Palonosetron is different serotonin receptor antagonists as it has a longer half-life (40 hours) and also a higher affinity for serotonin receptors. Single-dose regimen of palonosetron in combination with dexamethasone and aprepitant was found highly effective in preventing acute and delayed emesis following administration of moderately emetogenic chemotherapy.7
Steroids
Dexamethasone
Dexamethasone may also be used as monotherapy in low—emetic risk chemotherapy regimens. Glucocorticoids may act via the following mechanisms: (1) anti-inflammatory effect; (2) direct central action at the solitary tract nucleus, (3) interaction with the neurotransmitter serotonin, and receptor proteins tachykinin NK1 and NK2, alpha-adrenaline, etc.; (4) maintaining the normal physiological functions of organs and systems; (5) regulation of the hypothalamic-pituitary-adrenal axis; and (6) reducing pain and the concomitant use of opioids, which in turn reduces opioid-related nausea and vomiting.6 Dexamethasone, at intravenous doses of 10 to 20 mg, improved the efficacy of high-dose metoclopramide in cisplatin-treated patients by 20%.
Dopaminergic antagonists
Metoclopramide is a dopamine antagonist with a short-life and is one of the most frequently used dopamine antagonists. Metoclopramide is commonly used to treat nausea and vomiting associated with conditions such as uremia, radiation sickness, cancer and the effects of chemotherapy, A 10mg dose of metoclopramide has become the most commonly used dose.
Prochlorperazine is a piperazine phenothiazine antipsychotic which block postsynaptic mesolimbic dopaminergic receptors in the brain and has antiemetic effects by its antagonist actions in the D2 dopamine receptors in the chemoreceptor trigger zone. It also exhibits alpha-adrenergic blocking effect on α1 receptors and may depress the release of hypothalamic and hypophyseal hormones. 5 mg or 10 mg tablet 3 or 4 times daily. Daily dosages above 40 mg should be used only in resistant cases.
Perphenazine is a relatively high potency phenothiazine that blocks dopamine 2 (D2) receptors predominantly but also may possess antagonist actions at histamine 1 (H1) and cholinergic M1 and alpha 1 adrenergic receptors in the vomiting center leading to reduced nausea and vomiting. The potency of its antiemetic effects are intermediate. 8 to 16 mg daily in divided doses; 24 mg occasionally may be necessary; early dosage reduction is desirable.
Promethazine is a phenothiazine derivative which is also a potent histamine receptor H1 antagonist and an antiemetic. Its mechanisms of action include: blocking postsynaptic mesolimbic dopaminergic receptors in the brain; strong alpha-adrenergic blocking effects decreasing the release of hypothalamic and hypophyseal hormones; competing with histamine for the H1-receptor; muscarinic-blocking effects, and reducing stimuli to the brainstem reticular system. The antiemetic dose of promethazine is 12.5-25 mg every 4-6 hours as needed.
Trimethobenzamide is a (non-phenothiazine) benzamide antiemetic that acts centrally to block D2 receptors, thereby inhibiting the medullary chemoreceptor trigger zone by blocking emetic impulses to the vomiting center. The dose for nausea/vomiting is Oral: 300 mg 3-4 times/day, or I.M.: 200 mg 3-4 times/day, and for postoperative nausea and vomiting (PONV) is I.M.: 200 mg, followed 1 hour later by a second 200 mg dose.8
Nabilone, a cannabinoid, recently received Food and Drug Administration approval for the treatment of the nausea and vomiting in patients receiving cancer chemotherapy who fail to achieve adequate relief from conventional treatments. The cannabinoids exert antiemetic effects via agonism of cannabinoid receptors (CB1 and CB2). 1-2 mg orally 8-12 hourly. Nabilone is associated with significant adverse events and is not recommended as a first-line agent for CINV.
Dronabinol
Cannabinoid indicated in adults for the treatment of Nausea and vomiting associated with cancer chemotherapy in patients who have failed to respond adequately to conventional antiemetic treatments Dronabinol, the main psychoactive component in marijuana. Ingestion of high doses of dronabinol increases the risk of psychiatric adverse reactions if abused or misused, while continued administration can lead to addiction. The approved dosage of dronabinol is 5 mg/m2 orally 1 to 3 hours before the first dose of chemotherapy, and then every 2 to 4 hours after for a total of 6 doses. The dose may be increased in 2.5-mg/m2 increments to a maximum dose of 15 mg/m2.9
GABA mimetic
The anti-emetic mechanism of action of benzodiazepines, lorazepam, is related to the combination effects of sedation, reduction in anxiety, and possibly depression of the vomiting centre. 0.5 to 1 mg oral tablet by mouth once the night before chemotherapy, or the next day approximately one to two hours before chemotherapy.
The benzodiazepine midazolam is effective in prevention of postoperative vomiting. Midazolam given in combination with granisetron and dexamethasone waseffective in the treatment of acute nausea and vomiting after treatment with highly emetogenic chemotherapy in patients with vomiting refractory to antiemetic prophylaxis with granisetron and dexamethasone. IV midazolam 0.75mg/kg, was associated with significantly reduced PONV {Post operative nausea and vomiting}.
Antihistamine
Diphenhydramine or hydroxyzine in the prevention of CINV have not shown any anti-emetic activity. Antihistamines have a role in the treatment of nausea thought to be mediated by the vestibular system.10
Olanzapine
Olanzapine is an atypical antipsychotic agent of the thienobenzodiazepine class which acts as antagonist on multiple receptors including dopaminergic (D1, D2, D3, and D4), serotonergic (5-HT2A, 5-HT2C, 5-HT3, and 5-HT6), adrenergic (alpha1), histaminic (H1), and muscarinic (M1, M2, M3, and M4) receptors. Olanzapine has few extrapyramidal side effects because it has five times more affinity for 5HT2 receptors than for D2 receptors. The usual dose ranges between 2.5 and 30 mg once daily, but some studies report the use of the maximum dose of 60 mg per day depending on the symptomatology, the treatment response and the tolerance.11
Antiemetic choice
First-line antiemetic interventions
Three classes of antiemetic drugs,5 6 serotonin antagonists (e.g. ondansetron), corticosteroids (e.g. dexamethasone), and dopamine antagonists (e.g. droperidol) have similar efficacy against PONV, with a relative risk reduction of 25%. Three other serotonin antagonists, namely granisetron, dolasetron, and palonosetron, have a similar efficacy and side-effect profile (e.g. constipation, headache) to ondansetron.
Second-line antiemetic interventions
Metoclopramide is a widely used D2 antagonist. Contrary to popular belief, the 10 mg dose has no effect on PONV, but 25– 50 mg has similar efficacy compared with other antiemetics. Dimenhydrinate is an antihistamine like promethazine and cyclizine. There are few randomized controlled trials investigating its use for PONV. Transdermal scopolamine is a cholinergic antagonist typically used to treat motion sickness. A recent meta-analysis showed a 40% risk reduction in PONV.12
Antiemetic combinations
The combination of ondansetron plus dexamethasone or droperidol was significantly better than the combination of dexamethasone plus droperidol in the prophylaxis of postoperative nausea and vomiting in women undergoing general anesthesia for major gynecological surgery.
Netupitant/Palonosetron is a new option for the prevention of acute and delayed nausea and vomiting associated with highly emetogenic cisplatin-based chemotherapy or moderately emetogenic chemotherapy.
Ondansetron and dexamethasone reported better control of delayed vomiting using a combination of 4 mg ondansetron and 8 mg dexamethasone when compared with ondansetron alone.
Combination of granisetron plus droperidol with each agent alone in patients undergoing laparoscopic cholecystectomy and breast surgery.
The combination of ondansetron, dexamethasone and aprepitant is able to protect 66–78%of patients from emesis and 48–49% from nausea during the first cycle of cisplatin-basedchemotherapy.13, 14, 15
Herbal Remedies
Report of the beneficial effect of ginger as the rhizome of Zingiber officinale on motion sickness inspired a double-blind, randomized, cross-over study in which ginger 1 g/day for 4 days was noted to be superior to placebo in eliminating symptoms of hyperemesis gravidarum.
Conclusion
Antiemetic drugs have wide scope of activity by inhibiting various neurotransmitters and have therefore different ways to inhibit vomiting. Most of the severe cases require drug combination with other therapeutic class. Minimal effective doses of these combinations need to be established Side effects of drugs varies according to the therapeutic group. Antiemetics are not without adverse event profile hence dosage used should be according to severity and patients clinical profile.